Contoura® Vision
Contoura® Vision uses a proprietary
measurement system to create a unique map of
your eye’s surface, allowing a customized surgery
that will help you meet your vision goals.1,2
Contoura® Vision
Contoura® Vision uses a proprietary measurement system to create a unique map of your eye’s surface, allowing a customized surgery that will help you meet your vision goals.1,2
Who is a candidate for Contoura® Vision?
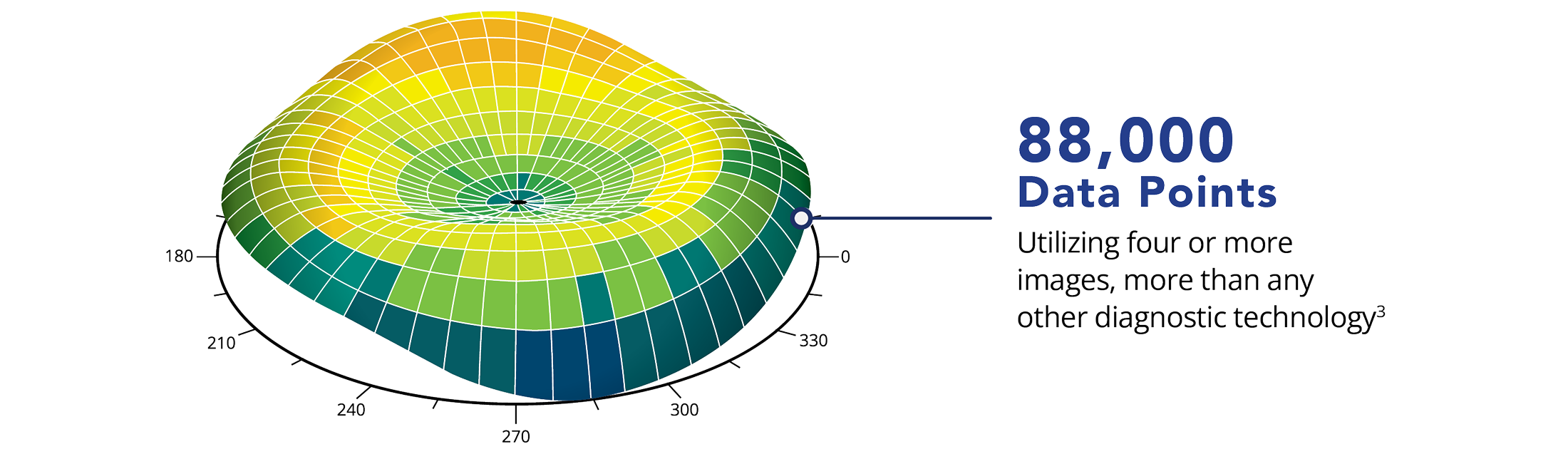
Contoura® Vision is a good option for people who want personalized laser vision correction. It captures 22,000 unique data points on the cornea of each eye, creating a unique topographic map of your eye to see the peaks and troughs of your cornea for a fully personalized procedure.3
You may be a good candidate if you:
- Have nearsightedness (myopia), with or without astigmatism4
- Have healthy eyes and no major corneal issues
- Want a treatment that maps and corrects the unique surface of your eye1,2,5,6
Schedule a consultation with an experienced LASIK surgeon to see if Contoura Vision is right for you.

Contoura® Vision provides a personalized approach to LASIK
Contoura® Vision can improve many of the visual symptoms commonly associated with glasses and contact lenses.2,7,8*

Difficulty Driving at Night

Glare
Starbursts

Halos
*vs. preoperative: glare p<0.01, halos p=0.01, night driving difficulty p<0.01, difficulty reading p<0.01, starbursts p=0.01, vision fluctuation p=0.03, light sensitivity p=0.03 (n=130 eyes).
How Contoura® Vision works
Just like your fingerprints, your eyes are unique to you.
Contoura® Vision is a good option for people who want personalized laser vision correction. It captures approximately 22,000 unique data points with each measurement of your eye's front surface, creating a unique topographic map of your eye. This allows your doctor to view the peaks and troughs of your cornea to assist in calculating your fully personalized procedure.3
What real Contoura® Vision patients are saying
Studies done to support FDA approval of Contoura® Vision LASIK demonstrated that:
93%
of Contoura® Vision patients achieved 20/20 vision without glasses or contact lenses9
At 12 months post-op; n=247
65%
of Contoura® Vision patients achieved 20/16 vision without glasses or contact lenses9
At 12 months post-op; n=274
98%
of patients would choose the Contoura® Vision procedure again9
At 12 months post-op; n=124
Frequently Asked Questions
Contoura® Vision is a customized LASIK treatment that uses a highly detailed scan of the eye’s surface — capturing up to 22,000 unique points — to create a personalized treatment plan.9,10
Unlike standard LASIK, which corrects vision based on your glasses prescription, Contoura® Vision uses LASIK technology and a proprietary measurement system to create a unique map of your eye’s surface, allowing your doctor to perform a personalized surgery that will improve your vision quality and help you meet your vision goals.1,2 Contoura-LASIK patients reported a reduction in side effects like glares and halos.7,8*
*vs. preoperative: glare p<0.01, halos p=0.01 (n=130 eyes).
In clinical studies, 93% of patients achieved 20/20 vision with Contoura® Vision.9 Patients reported significant decreases in glare, halos and difficulty driving at night, among other visual complaints.7,8* In fact, 65% of Contoura® Vision patients achieved 20/16 vision without glasses or contact lenses.9†
*vs. preoperative: glare p<0.01, halos p=0.01, night driving difficulty p<0.01, difficulty reading p<0.01, starbursts p=0.01, vision fluctuation p=0.03, light sensitivity p=0.03 (n=130 eyes).
†At 12 months post-operative (n=274).
Laser eye surgery is one of the most commonly performed procedures to correct refractive error.11 After surgery, many patients no longer require glasses or contact lenses to correct their vision and are very happy with their vision and quality of life.12 As with any surgical procedure, there are risk factors associated with laser eye surgery. Please consult your eye care professional to determine if this procedure is right for you. Reduced dependence on glasses or contact lenses is a potential benefit of laser eye surgery – individual patient results may vary.
Each person who undergoes laser eye surgery has a unique recovery experience. Many people are able to return to work the very next day. Others might experience a few minor side effects, such as watery or red eyes for a few days.
Yes—Contoura® Vision is a type of LASIK, which means the surgeon creates a thin flap in the outer layer of your cornea using a laser, to expose the underlying layer.12 The surgeon uses another laser to reshape the tissue of that layer using data specific to your eye.13 The flap is then placed back into position, where it naturally begins to heal.
This information pertains to all WaveLight® Excimer Laser Systems, including the WaveLight® ALLEGRETTO WAVE®, the ALLEGRETTOWAVE® Eye-Q, and the WaveLight® EX500.
Caution: Federal (U.S.) law restricts the WaveLight® Excimer Laser Systems to sale by or on the order of a physician. Only practitioners who are experienced in the medical management and surgical treatment of the cornea, who have been trained in laser refractive surgery (including laser calibration and operation) should use a WaveLight® Excimer Laser System. Indications: FDA has approved the WaveLight® Excimer Laser systems for use in laser-assisted in situ keratomileusis (LASIK) treatments for:
the reduction or elimination of myopia of up to - 12.00 D and up to 6.00 D of astigmatism at the spectacle plane;
the reduction or elimination of hyperopia up to + 6.00 D with and without astigmatic refractive errors up to 5.00 D at the spectacle plane, with a maximum manifest refraction spherical equivalent of + 6.00 D;
the reduction or elimination of naturally occurring mixed astigmatism of up to 6.00 D at the spectacle plane; and
the wavefront-guided reduction or elimination of myopia of up to -7.00 D and up to 3.00 D of astigmatism at the spectacle plane.
In addition, FDA has approved the WaveLight® ALLEGRETTO WAVE® Eye-Q Excimer Laser System, when used with the WaveLight® ALLEGRO Topolyzer® and topography-guided treatment planning software for topography-guided LASIK treatments for the reduction or elimination of up to -9.00 D of myopia, or for the reduction or elimination of myopia with astigmatism, with up to -8.00 D of myopia and up to 3.00D of astigmatism. The WaveLight® Excimer Laser Systems are only indicated for use in patients who are 18 years of age or older (21 years of age or older for mixed astigmatism) with documentation of a stable manifest refraction defined as ≤ 0.50 D of preoperative spherical equivalent shift over one year prior to surgery, exclusive of changes due to unmasking latent hyperopia.
Contraindications: The WaveLight® Excimer Laser Systems are contraindicated for use with patients who:
are pregnant or nursing;
have a diagnosed collagen vascular, autoimmune or immunodeficiency disease;
have been diagnosed keratoconus or if there are any clinical pictures suggestive of keratoconus;
are taking isotretinoin (Accutane*) and/or amiodarone hydrochloride (Cordarone*);
have severe dry eye;
have corneas too thin for LASIK;
have recurrent corneal erosion;
have advanced glaucoma; or
have uncontrolled diabetes.
Warnings: The WaveLight® Excimer Laser Systems are not recommended for use with patients who have:
systemic diseases likely to affect wound healing, such as connective tissue disease, insulin dependent diabetes, severe atopic disease or an immunocompromised status;
a history of Herpes simplex or Herpes zoster keratitis;
significant dry eye that is unresponsive to treatment;
severe allergies;
a history of glaucoma;
an unreliable preoperative wavefront examination that precludes wavefront-guided treatment; or
a poor quality preoperative topography map that precludes topography-guided LASIK treatment.
The wavefront-guided LASIK procedure requires accurate and reliable data from the wavefront examination. Every step of every wavefront measurement that may be used as the basis for a wavefrontguided LASIK procedure must be validated by the user. Inaccurate or unreliable data from the wavefront examination will lead to an inaccurate treatment.
Topography-guided LASIK requires preoperative topography maps of sufficient quality to use for planning a topography-guided LASIK treatment. Poor quality topography maps may affect the accuracy of the topography-guided LASIK treatment and may result in poor vision after topography-guided LASIK.
Precautions: The safety and effectiveness of the WaveLight® Excimer Laser Systems have not been established for patients with:
progressive myopia, hyperopia, astigmatism and/or mixed astigmatism, ocular disease, previous corneal or intraocular surgery, or trauma in the ablation zone;
corneal abnormalities including, but not limited to, scars, irregular astigmatism and corneal warpage;
residual corneal thickness after ablation of less than 250 microns due to the increased risk for corneal ectasia;
pupil size below 7.0 mm after mydriatics where applied for wavefront-guided ablation planning;
history of glaucoma or ocular hypertension of > 23 mmHg;
taking the medications sumatriptan succinate (Imitrex*);
corneal, lens and/or vitreous opacities including, but not limited to cataract;
iris problems including, but not limited to, coloboma and previous iris surgery compromising proper eye tracking; or
taking medications likely to affect wound healing including (but not limited to) antimetabolites.
In addition, safety and effectiveness of the WaveLight® Excimer Laser Systems have not been established for:
treatments with an optical zone < 6.0 mm or > 6.5 mm in diameter, or an ablation zone > 9.0 mm in diameter; or
wavefront-guided treatment targets different from emmetropia (plano) in which the wavefront calculated defocus (spherical term) has been adjusted; In the WaveLight® Excimer Laser System clinical studies, there were few subjects with cylinder amounts > 4 D and ≤ 6 D. Not all complications, adverse events, and levels of effectiveness may have been determined for this population. Pupil sizes should be evaluated under mesopic illumination conditions. Effects of treatment on vision under poor illumination cannot be predicted prior to surgery.
Adverse Events and Complications
Myopia: In the myopia clinical study, 0.2% (2/876) of the eyes had a lost, misplaced, or misaligned flap reported at the 1 month examination. The following complications were reported 6 months after LASIK: 0.9% (7/818) had ghosting or double images in the operative eye; 0.1% (1/818) of the eyes had a corneal epithelial defect.
Hyperopia: In the hyperopia clinical study, 0.4% (1/276) of the eyes had a retinal detachment or retinal vascular accident reported at the 3 month examination. The following complications were reported 6 months after LASIK: 0.8% (2/262) of the eyes had a corneal epithelial defect and 0.8% (2/262) had any epithelium in the interface.
Mixed Astigmatism: In the mixed astigmatism clinical study, two adverse events were reported. The first event involved a patient who postoperatively was subject to blunt trauma to the treatment eye 6 days after surgery. The patient was found to have an intact globe with no rupture, inflammation or any dislodgement of the flap. UCVA was decreased due to this event. The second event involved the treatment of an incorrect axis of astigmatism. The axis was treated at 60 degrees instead of 160 degrees. The following complications were reported 6 months after LASIK: 1.8% (2/111) of the eyes had ghosting or double images in the operative eye. Wavefront-Guided Myopia: The wavefront-guided myopia clinical study included 374 eyes treated; 188 with wavefront-guided LASIK (Study Cohort) and 186 with Wavefront Optimized® LASIK (Control Cohort). No adverse events occurred during the postoperative period of the wavefront-guided LASIK procedures. In the Control Cohort, one subject undergoing traditional LASIK had the axis of astigmatism programmed as 115 degrees instead of the actual 155 degree axis. This led to cylinder in the left eye. The following complications were reported 6 months after wavefront guided LASIK in the Study Cohort: 1.2% (2/166) of the eyes had a corneal epithelial defect; 1.2% (2/166) had foreign body sensation; and 0.6% (1/166) had pain. No complications were reported in the Control Cohort. Topography-Guided Myopia: There were six adverse events reported in the topography-guided myopia study. Four of the eyes experienced transient or temporary decreases in vision prior to the final 12 month follow-up visit, all of which were resolved by the final followup visit. One subject suffered from decreased vision in the treated eye, following blunt force trauma 4 days after surgery. One subject experienced retinal detachment, which was concluded to be unrelated to the surgical procedure.
Clinical Data
Myopia: The myopia clinical study included 901 eyes treated, of which 813 of 866 eligible eyes were followed for 12 months. Accountability at 3 months was 93.8%, at 6 months was 91.9%, and at 12 months was 93.9%. Of the 782 eyes that were eligible for the uncorrected visual acuity (UCVA) analysis of effectiveness at the 6-month stability time point, 98.3% were corrected to 20/40 or better, and 87.7% were corrected to 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: visual fluctuations (28.6% vs. 12.8% at baseline). Long term risks of LASIK for myopia with and without astigmatism have not been studied beyond 12 months.
Hyperopia: The hyperopia clinical study included 290 eyes treated, of which 100 of 290 eligible eyes were followed for 12 months. Accountability at 3 months was 95.2%, at 6 months was 93.9%, and at 12 months was 69.9%. Of the 212 eyes that were eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 95.3% were corrected to 20/40 or better, and 69.4% were corrected to 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms as “much worse” at 6 months post-treatment: halos (6.4%); visual fluctuations (6.1%); light sensitivity (4.9%); night driving glare (4.2%); and glare from bright lights (3.0%). Long term risks of LASIK for hyperopia with and without astigmatism have not been studied beyond 12 months.
Mixed Astigmatism: The mixed astigmatism clinical study included 162 eyes treated, of which 111 were eligible to be followed for 6 months. Accountability at 1 month was 99.4%, at 3 months was 96.0%, and at 6 months was 100.0%. Of the 142 eyes that were eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 97.3% achieved acuity of 20/40 or better, and 69.4% achieved acuity of 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: sensitivity to light (52.9% vs. 43.3% at baseline); visual fluctuations (43.0% vs. 32.1% at baseline); and halos (42.3% vs. 37.0% at baseline). Long term risks of LASIK for mixed astigmatism have not been studied beyond 6 months.
Wavefront-Guided Myopia: The wavefront-guided myopia clinical study included 374 eyes treated; 188 with wavefront-guided LASIK (Study Cohort) and 186 with Wavefront Optimized® LASIK (Control Cohort). 166 of the Study Cohort and 166 of the Control Cohort were eligible to be followed at 6 months. In the Study Cohort, accountability at 1 month was 96.8%, at 3 months was 96.8%, and at 6 months was 93.3%. In the Control Cohort, accountability at 1 month was 94.6%, at 3 months was 94.6%, and at 6 months was 92.2%. Of the 166 eyes in the Study Cohort that were eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 99.4% were corrected to 20/40 or better, and 93.4% were corrected to 20/20 or better. Of the 166 eyes in the Control Cohort eligible for the UCVA analysis of effectiveness at the 6-month stability time point, 99.4% were corrected to 20/40 or better, and 92.8% were corrected to 20/20. In the Study Cohort, subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms at a “moderate” or “severe” level at least 1% higher at 3 months post-treatment than at baseline: light sensitivity (47.8% vs. 37.2% at baseline) and visual fluctuations (20.0% vs. 13.8% at baseline).
In the Control Cohort, the following visual symptoms were reported at a “moderate” or “severe” level at least 1% higher at 3 months post treatment than at baseline: halos (45.4% vs. 36.6% at baseline) and visual fluctuations (21.9% vs. 18.3% at baseline). Long term risks of wavefront-guided LASIK for myopia with and without astigmatism have not been studied beyond 6 months. Topography-Guided Myopia: The topography-guided myopia clinical study included 249 eyes treated, of which 230 eyes were followed for 12 months. Accountability at 3 months was 99.2%, at 6 months was 98.0%, and at 12 months was 92.4%. Of the 247 eyes that were eligible for the UCVA analysis at the 3-month stability time point, 99.2% were corrected to 20/40 or better, and 92.7% were corrected to 20/20 or better. Subjects who responded to a patient satisfaction questionnaire before and after LASIK reported the following visual symptoms as “marked” or “severe” at an incidence greater than 5% at 1 month after surgery: dryness (7% vs. 4% at baseline) and light sensitivity (7% vs. 5% at baseline). Visual symptoms continued to improve with time, and none of the visual symptoms were rated as being “marked” or “severe” with an incidence of at least 5% at 3 months or later after surgery. Long term risks of topography-guided LASIK for myopia with and without astigmatism have not been studied beyond 12 months. Information for Patients: Prior to undergoing LASIK surgery with a WaveLight® Excimer Laser System, prospective patients must receive a copy of the relevant Patient Information Booklet, and must be informed of the alternatives for correcting their vision, including (but not limited to) eyeglasses, contact lenses, photorefractive keratectomy, and other refractive surgeries.
Attention: Please refer to a current WaveLight® Excimer Laser System Procedure Manual for a complete listing of the indications, complications, warnings, precautions, and side effects.
*Trademarks are property of their respective owners.
References:
1. Ozulken F, Yuksel E Tekin K, et al. Comparison of wavefront-optimized ablation and topography-guided Contoura® ablation with LYRA protocol in LASIK. J Refract Surg. 2019;35(4):222–229.
2. Brunson P, Mann PM II, Mann PM, Potvin R. Comparison of refractive and visual acuity results after Contoura® Vision topography-guided LASIK planned with the Phorcides Analytic Engine to results after wavefront-optimized LASIK in eyes with oblique astigmatism. PLoS ONE. 2022;17(12):e0279357.
3. Wavelight ALLEGRO Topolyzer VARIO User Manual.
4. Stulting RD, Fant BS; T-CAT Study Group. Results of topography-guided laser in situ keratomileusis custom ablation treatment with a refractive excimer laser. J Cataract Refract Surg. 2016;42(1):11–18.
5. Wavelight InnovEyes™ Sightmap Diagnostic Device User Manual. 2018.
6. Alcon Data on File, 2021. [REF-18191]
7. Stulting RD, Lobanoff M, Mann PM 2nd, Wexler S, Stonecipher K, Potvin R. Clinical and refractive outcomes after topography-guided refractive surgery planned using Phorcides surgery planning software. J Cataract Refract Surg. 2022;48(9):1010–1015.
8. Rush SW, Pickett CJ, Wilson BJ, Rush RB. Topography-Guided LASIK: A Prospective Study Evaluating Patient-Reported Outcomes. Clin Ophthalmol. 2023;17:2815–2824.
9. FDA Summary of Safety and Effectiveness Data. ALLEGRETTO WAVE Eye-Q Excimer Laser.
10. Lobanoff M, Stonecipher K, Tooma T, Wexler S, Potvin R. Clinical outcomes after topography-guided LASIK: comparing results based on a new topography analysis algorithm with those based on manifest refraction. J Cataract Refract Surg. 2020;46(6):814–819.
11. Mayo Clinic. LASIK Eye Surgery. Accessed May 3, 2022. Accessed from: https://www.mayoclinic. org/tests-procedures/lasik-eye-surgery/about/pac-20384774
12. Bastawrous A, Silvester A, Batterbury M. Laser refractive eye surgery. BMJ. 2011;342:d2345.
13. Quick Procedure Manual EX500 en Rev.06 2017-11-17.
Please refer to relevant product directions for use for complete list of indications, contraindications, and warnings. Consult your doctor on relevant safety information about the treatment.