MyAlcon | Sweden
This page is available in English. Please click below for other locations.
The TFOS DEWS II® and Recommendations
Multiple aspects of Dry Eye disease

The most widely recognized definition of Dry Eye disease was created by the TFOS DEWS II® Definition and Classification Subcommittee as an evidence-based definition and a contemporary classification system for Dry Eye disease.
The report involved the efforts of 150 clinical and basic science research experts from around the world, who utilized an evidence-based approach and process. Below we’ve given you the outline of some of the report’s key learnings.
We believe these key points can assist you to better understand Dry Eye disease and help identify the patients’ tear deficiency, ultimately helping you find the right solution for them. As by relieving Dry Eye symptoms, the progression of the symptoms and signs can be reduced.
The TFOS DEWS II® definition of Dry Eye
Dry Eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film, and accompanied by ocular symptoms, in which tear film instability and hyperosmolarity, ocular surface inflammation and damage, and neurosensory abnormalities play etiological roles1. Healthy tears are an important part of overall eye health and vision. The TFOS DEWS II® suggests there are 2 key layers that we should consider when it comes to identifying the patient’s tear deficiency.
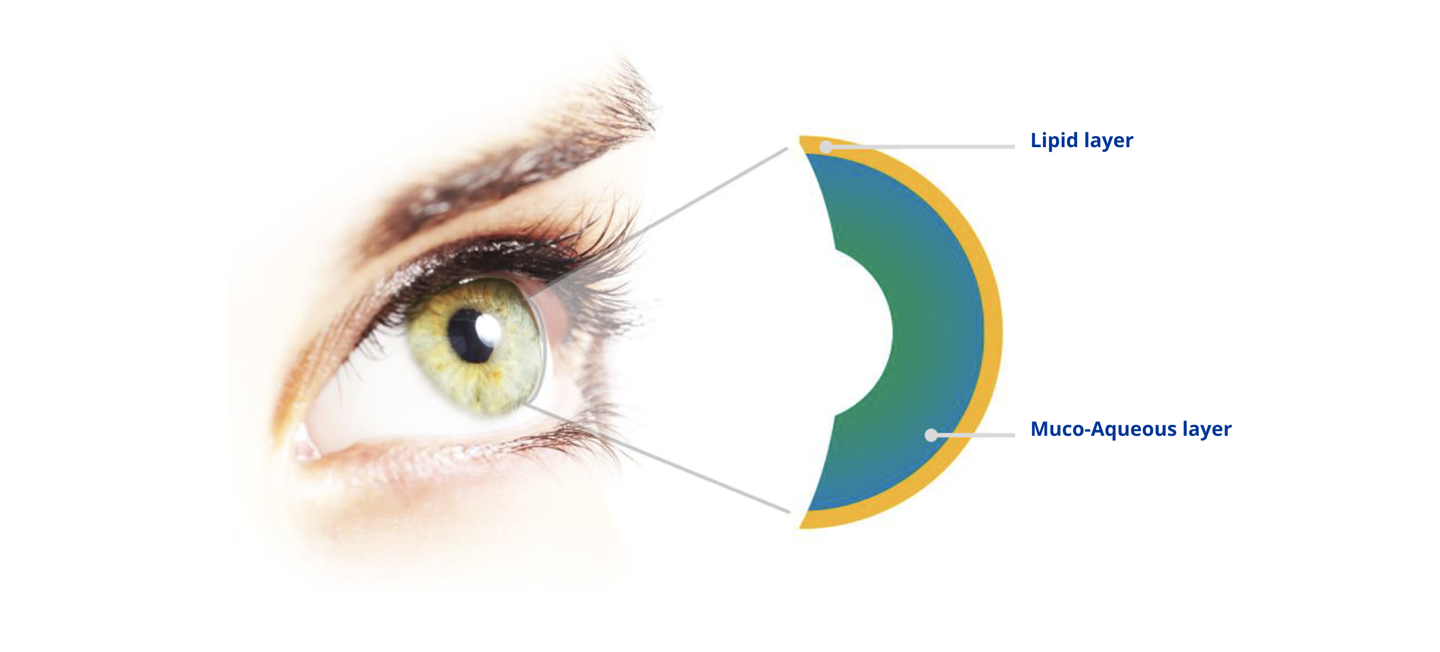
1) Lipid Layer2: Protects and maintains tear film stability and works with the muco-aqueous layer to prevent evaporation and collapse.
2) Muco-Aqueous Layer3: Hydrates, nourishes, and protects the ocular surface. Helps spread and stabilize the tear film, lubricates the ocular surface, and protects against pathogens.
There are 3 types of Dry Eye:

- Acqueous-deficient Dry Eye In aqueous-deficient Dry Eye, tear hyperosmolarity results from reduced lacrimal secretion (with normal evaporation)4
- Evaporative Dry Eye In evaporative Dry Eye, tear hyperosmolarity is caused by excessive evaporation, with normal lacrimal gland function (typically due to meibomian gland dysfunction [MGD])4
- Aqueous-deficient and evaporative Dry Eye are non-mutually exclusive AS Dry Eye progresses, it is increasingly likely that patients will exhibit characteristics of both types5
The Vicious Circle
Meibomian gland dysfunction (MGD) is the most frequent cause of dry eye disease (DED). The pathogenesis of both MGD and DED can be described in terms of a ‘vicious circle’: the underlying pathophysiological mechanisms of DED and MGD interact, resulting in a double vicious circle. The MGD vicious circle is self-stimulated by microbiological changes, which results in increased melting temperature of meibum and subsequent meibomian gland blockage, reinforcing the vicious circle of MGD. Meibomian gland blockage, dropout and inflammation directly link the two vicious circles. MGD associated tear film instability provides an entry point into the vicious circle of DED and leads to hyperosmolarity and inflammation, which are both a cause and consequence of DED.
As such, DED may be described as an autonomous self-sustaining disease state that is progressively disconnected from its initial causes. In the vicious circle, rapid break-up of the tear film after blinking (tear film instability) leads to local drying and hyperosmolarity of the epithelial surface. In turn, this leads to apoptosis, inflammation and a loss of mucin-producing goblet cells. This cascade of mechanisms, involving osmotic, mechanical and inflammatory stress, destroys goblet cells and defence systems of the ocular surface leading to further damage of the tear film, and thus closes the circle.
Other factors such as corneal surgery, low humidity and high airflow, contact lens wear, allergies or preservatives may disrupt reflex tear delivery to the ocular surface or increase tear film instability, thus initiating entry into the vicious circle6.
The vicious circle scheme7 allows us to understand why, once the cycle is initiated, the continuous environmental challenge acting on a compromised ocular surface allows the vicious circle to perpetuate, even if the initial cause has been removed or reduced. The vicious circle scheme may also promote the development of therapeutic strategies that can simultaneously target the multiple mechanisms underlying the pathophysiology of DED.8 For example, tear substitutes with osmoprotective properties9-11 may act on multiple points to break the vicious circle of DED.9,11,12 Topical anti-inflammatory strategies, such as those containing steroids or cyclosporine, target inflammation and help halt the cycle.13,14
Thus, a better understanding of the vicious circle may improve DED management with existing therapies and could also aid in the development of new therapies.

References:
1. Craig JP, et al., TFOS DEWS II Report Executive Summary, The Ocular Surface (2017), ttp://dx.doi.org/10.1016/ j.jtos.2017.08.003.
2. Perry HD. Dry eye disease: pathophysiology, classification, and diagnosis. Am J Manag Care. 2008;14(3 suppl):S79-S87.
3. Lemp MA, Crews LA, Bron AJ, Foulks GN, Sullivan BD. Distribution of aqueous-deficient and evaporative dry eye in a clinic-based patient cohort: a retrospective study. Cornea. 2012;31(5):472–478.
4. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017;15:802-812.
5. Craig JP, Nichols KK, Akpek EK, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017;15:276-283.
6. International Dry Eye Workshop. Report of the International Dry Eye Workshop (DEWS). Ocul Surf 2007;5:61–204.
7. Baudouin et al, Role Of Hyperosmolarity In The Pathogenesis And Management Of Dry Eye Disease: Proceedings Of The Ocean Group Meeting, The Ocular Surface / October 2013, VOL. 11 NO. 4 / www.theocularsurface.com.
8. Labetoulle M, Baudouin C. From pathogenic considerations to a simplified decision-making schema in dry eye disease. J Fr Ophtalmol 2013;36:543–7.
9. Baudouin C, Aragona P, Messmer EM, et al. Role of hyperosmolarity in the pathogenesis and management of dry eye disease:
10. Hamano T, Horimoto K, Lee M, et al. Sodium hyaluronate eyedrops enhance tear film stability. Jpn J Ophthalmol 1996;40:62–5.
11. Simmons PA, Chang-Lin J-E, Chung Q, et al. Effect of compatible solutes on transepithelial electrical resistance and uptake in primary rabbit corneal epithelial cell layers model. Presented at the Association for Research in Vision and Ophthalmology (ARVO), 2007.
12. Bayhan SA, Bayhan HA, Muhafiz E, et al. Effects of osmoprotective eye drops on tear osmolarity in contact lens wearers. Can J Ophthalmol 2015;50:283–9.
13. Geerling G, Tauber J, Baudouin C, et al. The International Workshop on Meibomian Gland Dysfunction: report of the Subcommittee on Management and Treatment of Meibomian Gland Dysfunction. Invest Ophthalmol Vis Sci 2011;52:2050–64.
14. Qiao J, Yan X. Emerging treatment options for meibomian gland dysfunction. Clin Ophthalmol 2013;7:1797–803.
See instruction for use, precautions, warnings, contraindications and adverse effects.