Clareon® Toric IOL
Beyond stability, the difference is material.
Clareon® Collection IOLs
More options for more patients: four optic designs, one glistening-free* material1,2
Clareon® Toric IOLs provide exceptional clarity1,2*, allowing you to confidently deliver the long-lasting refractive outcomes that your patients expect.
Exceptional Clarity that Lasts1,2†
Delivers among the lowest levels of glistenings, SSNGs, and surface haze.2-4† In long-term clinical studies, Clareon® IOLs were reported as glistening-free over 3 and 9 years.2-4†
Proprietary Precision Edge Design1,5
Proprietary edge curvature designed to help reduce PCO and edge glare.1,5
Superior Axial Stability6,7
Fibronectin helps bind the material to the capsule, anchoring the lens in place to help reduce PCO and improve stability.5-8
Optical Design with Proven Performance9
Clareon® and AcrySof® share the same -0.2µm aspheric design resulting in improved depth of focus with a fully usable 6mm optic.9††
See the difference with the Clareon® Toric IOL
The Clareon® Toric IOL utilizes a new hydrophobic acrylic BioMaterial and advanced manufacturing process to deliver a pristine IOL.1-4
Stableforce® haptics provide a biomechanical advantage
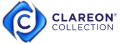
Clareon® Toric IOLs deliver the rotational stability you expect from the very beginning.10
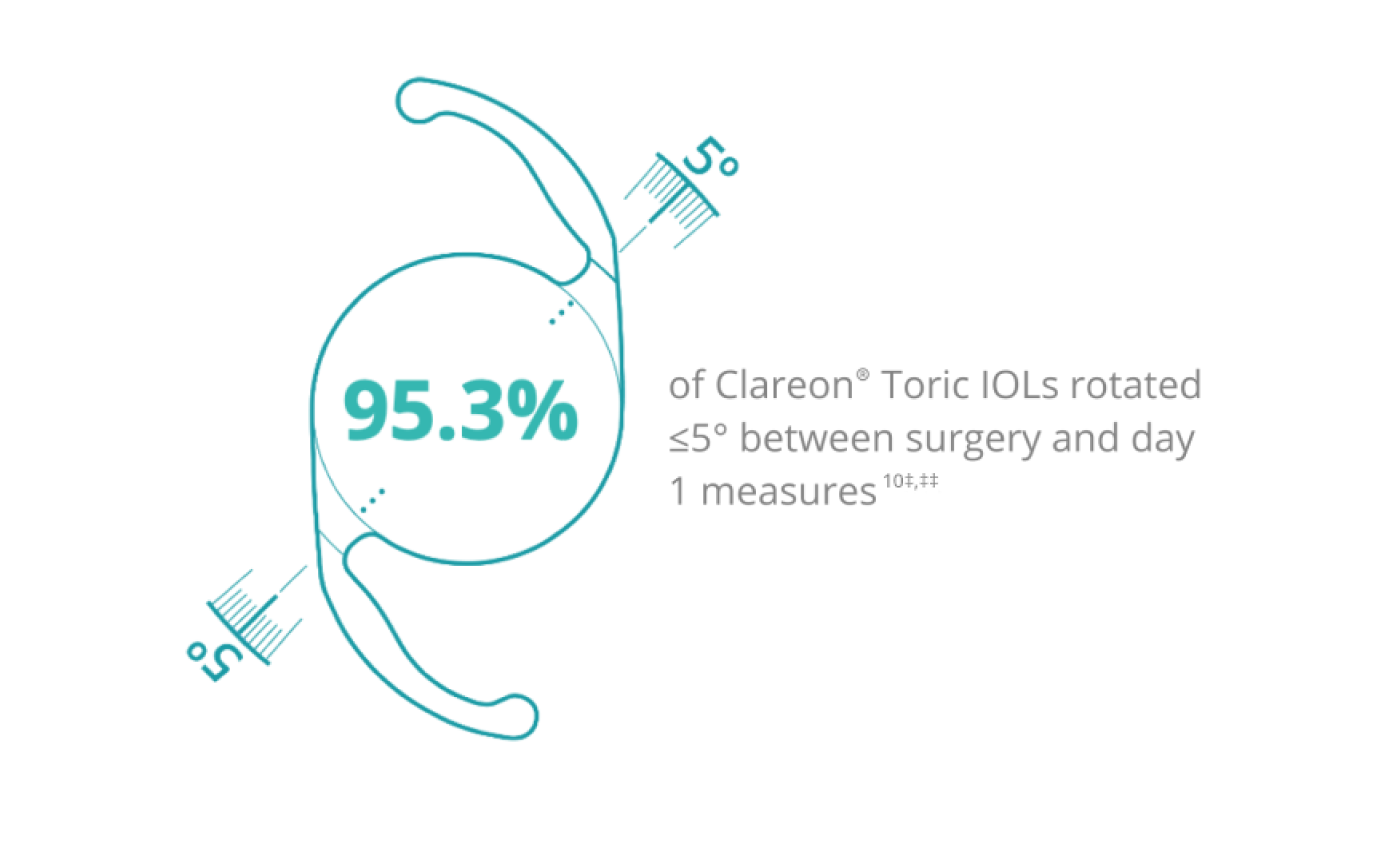
‡ In an additional analysis, 98.4% of Clareon® IOLs (n=127 ) had an absolute rotation of ≤10° between surgery and 6 months.
‡‡ Mean rotation at day 1 (n=127 ) and 6 months (n=124 ): 1 .8° ± 3 .7° and 2 .3° ± 3 .9°, respectively. Study measures were taken at baseline (immediately after surgery, <1 hour ), at day 1, and at months 1, 3, and 6.
of AcrySof® IQ Toric IOLs were ≤5° of post-op alignment11§,§§
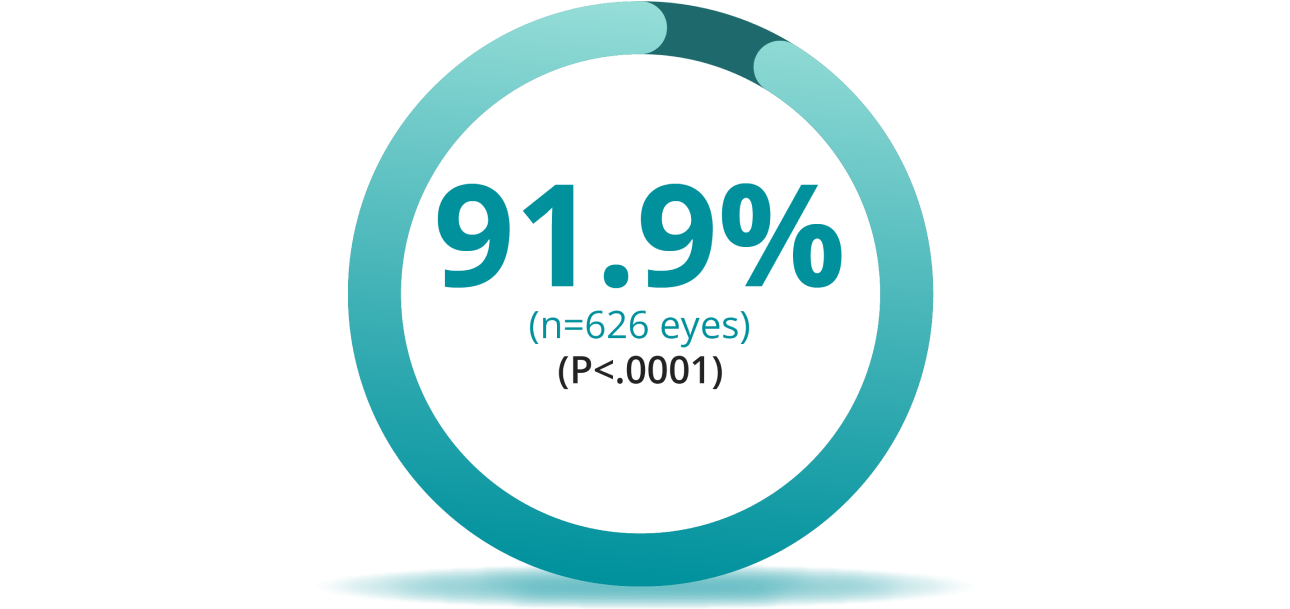
§ Mean absolute difference between achieved lens axis at surgery and visit 5 (12 months), ±5.8˚.
§§ AstigmatismFix.com is an online calculator to help surgeons determine if a previously placed toric IOL is ideally aligned. The analysis dataset includes 5,674 entries, with each unique lens and intended orientation identified, in addition to postoperative IOL orientation. ≥ 5° from intended axis. The dataset was weighted based on the estimated market usage of each lens. The full evaluation included AcrySof® IQ Toric, TECNIS^ Toric, Trulign^ Toric and Staar^ Toric IOLs.
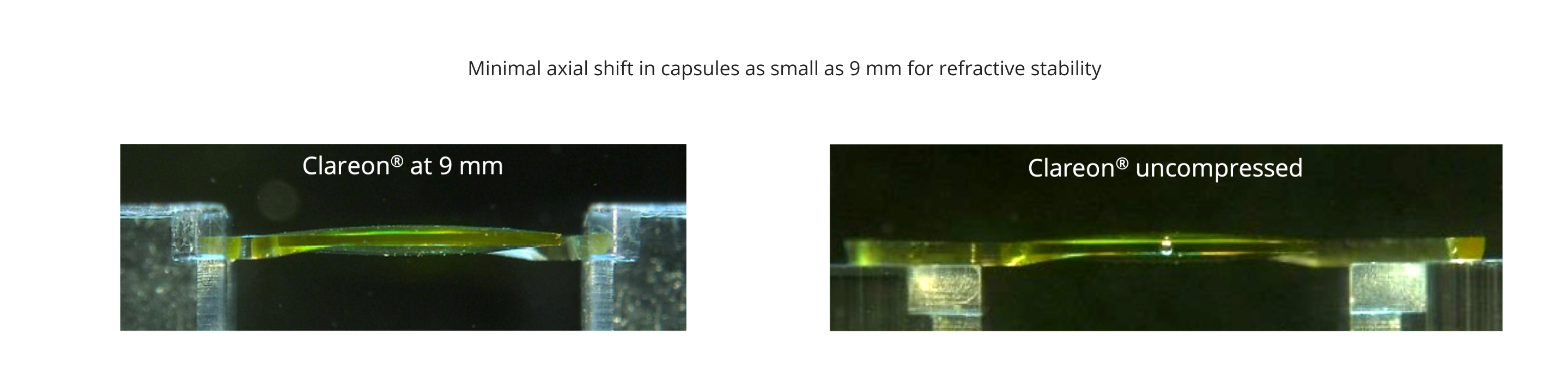
Exceptional axial stability6,7 for a range of capsule sizes
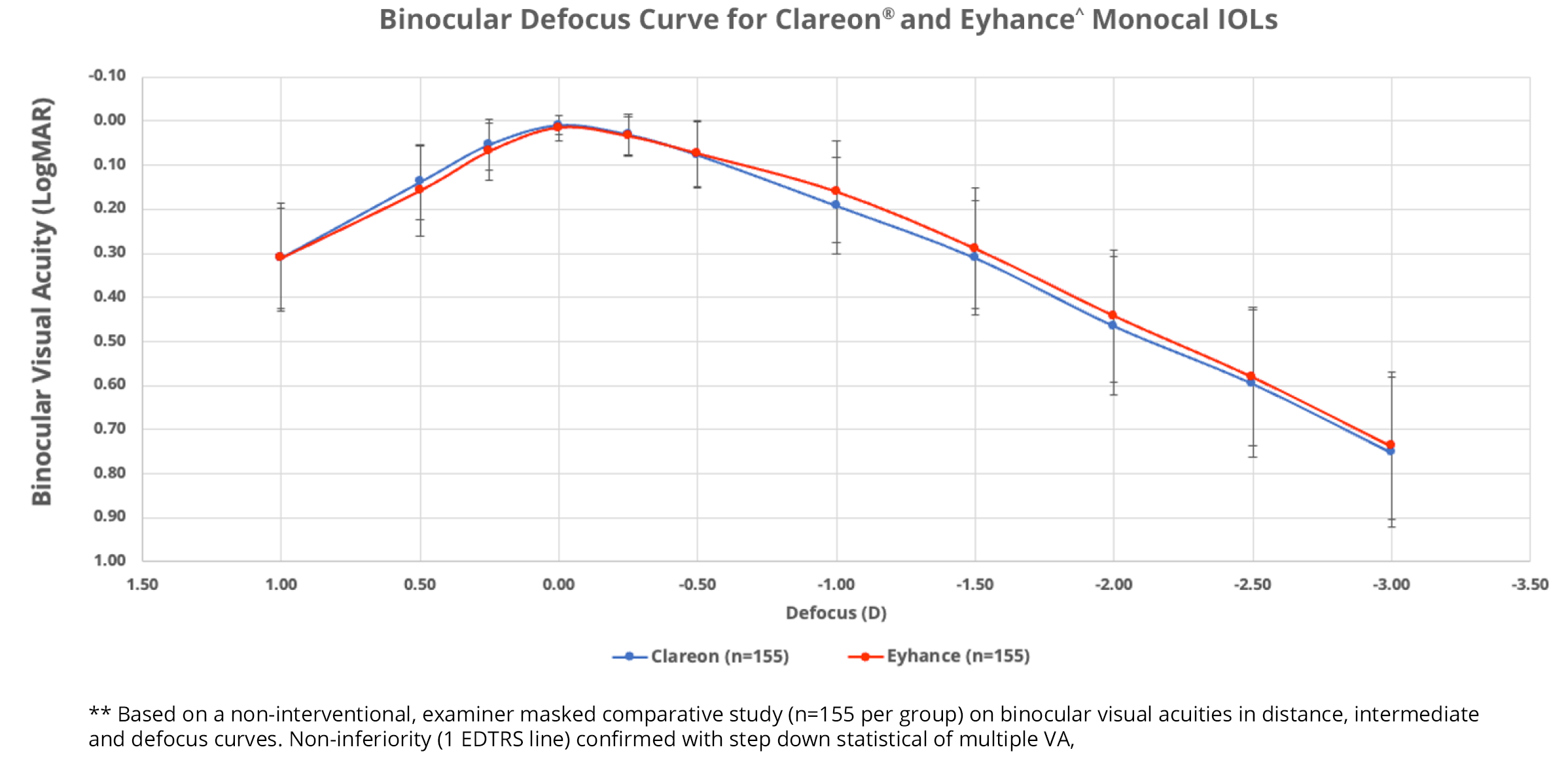
No significant difference in range of vision was observed between Clareon® and Eyhance^ monofocals
In a clinical study of 310 patients (155 per group), Clareon® and Eyhance^ IOLs offered comparable binocular range of vision12**
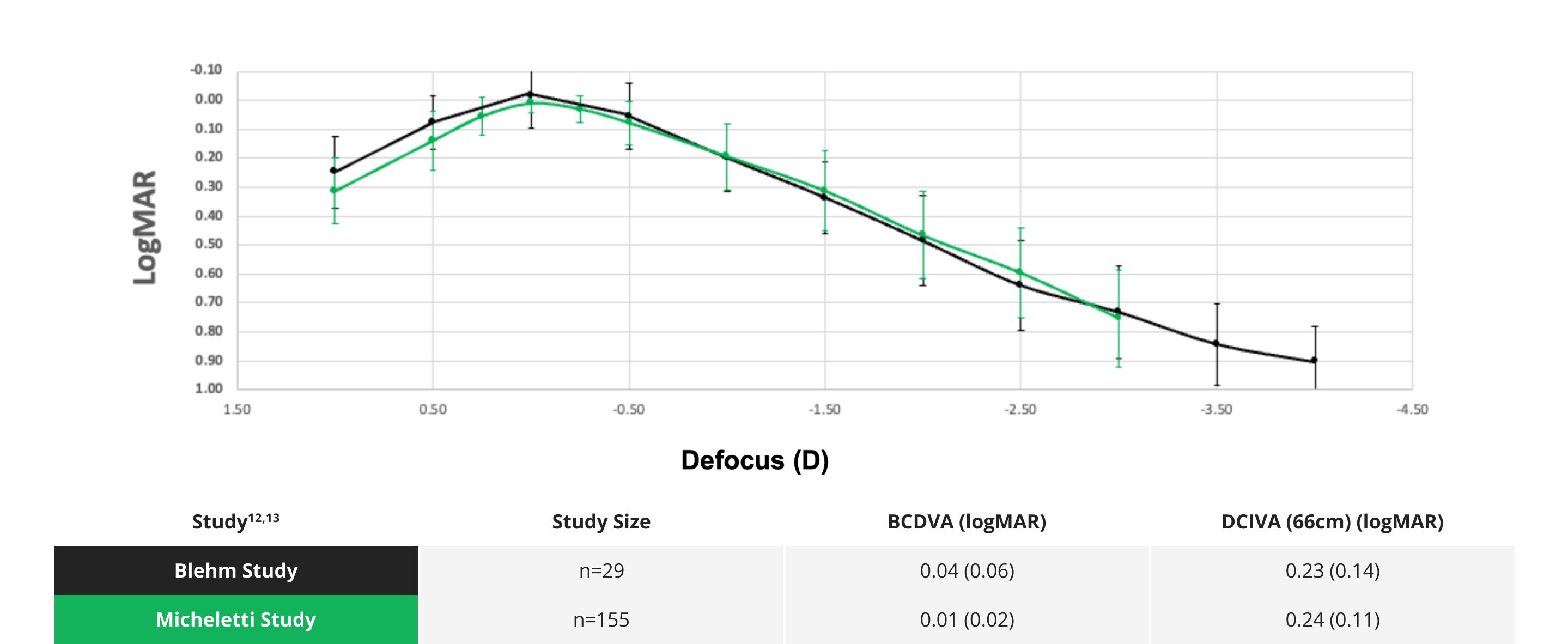
Clareon® IOLs: Consistent outcomes you can trust
Based on two studies with a total of 184 patients, Clareon® IOLs deliver predictable range of vision while maintaining 20/20 visual acuity at distance12,13
Explore additional resources for the Clareon® Toric IOLs
The Clareon® collection provides more options for your astigmatic patients than any other platform in its class


Clareon® Monofocal Toric
Glistening-free† BioMaterial with outstanding rotational stability and predictable placement.2-4,6,7


Clareon® PanOptix® Toric
The first and only trifocal lens in the United States, offering a full range of vision and exceptional clarity.1,14*


Clareon® Vivity® Toric
The first and only non-diffractive presbyopia-mitigating IOL with exceptional clarity*, excellent intermediate vision, and functional near vision.1,15
Alcon online Clareon® Toric IOL calculator with the Barrett Algorithm

Share our product brochure with your patients to communicate the Clareon® difference
Available on Clareon®: Alcon’s most advanced IOL biomaterial to date

* Based on in vitro examinations of glistenings, surface haze and SSNGs.
† Defined as modified Miyata grade 0, <25mv /mm2 over 3 years (n=138 ), and over 9 years (n=20 ), respectively.
†† Clareon® and AcrySof® share the same -0.2μm aspheric design resulting in improved depth of focus.
^ Trademarks are the property of their respective owners.
IMPORTATN PRODUCT INFORMATION - CLAREON® ASPHERIC FAMILY OF HYDROPHOBIC ACRYLIC IOLS
CAUTION: Restricted by law to sale by or on the order of a physician.
INDICATIONS: The family of Clareon® intraocular lenses (IOLs) includes the Clareon® Aspheric Hydrophobic Acrylic and Clareon® Aspheric Toric IOLs, the Clareon® PanOptix® Trifocal Hydrophobic IOL, Clareon® PanOptix® Toric, Clareon® Vivity® Extended Vision Hydrophobic Posterior Chamber IOL and Clareon® Vivity® Toric IOLs. Each of these IOLs is indicated for visual correction of aphakia in adult patients following cataract surgery. In addition, the Clareon® Toric IOLs are indicated to correct pre-existing corneal astigmatism at the time of cataract surgery. The Clareon® PanOptix® lens mitigates the effects of presbyopia by providing improved intermediate and near visual acuity, while maintaining comparable distance visual acuity with a reduced need for eyeglasses, compared to a monofocal IOL. The Clareon® Vivity® lens mitigates the effects of presbyopia by providing an extended depth of focus. Compared to an aspheric monofocal IOL, the lens provides improved intermediate and near visual acuity, while maintaining comparable distance visual acuity. All of these IOLs are intended for placement in the capsular bag.
WARNINGS / PRECAUTIONS: General cautions for all Clareon® IOLs: Careful preoperative evaluation and sound clinical judgment should be used by the surgeon to decide the risk/benefit ratio before implanting any IOL in a patient with any of the conditions described in the Directions for Use that accompany each IOL. Physicians should target emmetropia, and ensure that IOL centration is achieved.
For the Clareon® Aspheric Toric, PanOptix® Toric and Vivity® Toric IOLs, the lens should not be implanted if the posterior capsule is ruptured, if the zonules are damaged, or if a primary posterior capsulotomy is planned. Rotation can reduce astigmatic correction; if necessary lens repositioning should occur as early as possible prior to lens encapsulation.
For the Clareon® PanOptix® IOL, some visual effects may be expected due to the superposition of focused and unfocused multiple images. These may include some perceptions of halos or starbursts, as well as other visual symptoms. As with other multifocal IOLs, there is a possibility that visual symptoms may be significant enough that the patient will request explant of the multifocal IOL. A reduction in contrast sensitivity as compared to a monofocal IOL may be experienced by some patients and may be more prevalent in low lighting conditions. Therefore, patients implanted with multifocal IOLs should exercise caution when driving at night or in poor visibility conditions. Patients should be advised that unexpected outcomes could lead to continued spectacle dependence or the need for secondary surgical intervention (e.g., intraocular lens replacement or repositioning). As with other multifocal IOLs, patients may need glasses when reading small print or looking at small objects. Posterior capsule opacification (PCO), may significantly affect the vision of patients with multifocal IOLs sooner in its progression than patients with monofocal IOLs.
For the Clareon® Vivity® IOL, most patients implanted with the Vivity® IOL are likely to experience significant loss of contrast sensitivity as compared to a monofocal IOL. Therefore, it is essential that prospective patients be fully informed of this risk before giving their consent for implantation of the Clareon® Vivity® IOL. In addition, patients should be warned that they will need to exercise caution when engaging in activities that require good vision in dimly lit environments, such as driving at night or in poor visibility conditions, especially in the presence of oncoming traffic. It is possible to experience very bothersome visual disturbances, significant enough that the patient could request explant of the IOL. In the parent AcrySof® IQ Vivity® IOL clinical study, 1% to 2% of AcrySof® IQ Vivity® IOL patients reported very bothersome starbursts, halos, blurred vision, or dark area visual disturbances; however, no explants were reported.
Prior to surgery, physicians should provide prospective patients with a copy of the Patient Information Brochure available from Alcon informing them of possible risks and benefits associated with these IOLs.
ATTENTION: Reference the Directions for Use labeling for each IOL for a complete listing of indications, warnings and precautions.
REFERENCES:
- Clareon® Toric Directions for Use.
- Werner L, Thatthamla I, Ong M, et al. Evaluation of clarity characteristics in a new hydrophobic acrylic IOL. J Cataract Refract Surg. 2019;45:1490-1497.
- Oshika T, Fujita Y, Inamura M, Miyata K. Mid-term and long-term clinical assessments of a new 1-piece hydrophobic acrylic IOL with hydroxyethyl meth-acrylate. J Cataract Refract Surg. 2020 May;46(5):682-687.
- Maxwell A, Suryakumar R. Long-term effectiveness and safety of a three-piece acrylic hydrophobic intraocular lens modified with hydroxyethyl-methacrylate: an open-label, 3-year follow-up study. Clin Ophthalmol. 2018;12:2031-2037.
- Das KK, Werner L, Collins S, Hong X. In vitro and schematic model eye assessment of glare or positive dysphotopsia-type photic phenomena: Comparison of a new material IOL to other monofocal IOLs. J Cataract Refract Surg. 2019;45(2):219-227.
- Alcon Data on File, 2017.
- Lane S, Collins S, Das KK, Maass S, Thatthamla I, Schatz H, Van Noy S, Jain R. Evaluation of intraocular lens mechanical stability. J Cataract Refract Surg. 2019 Apr;45(4):501-506.
- Alcon data on file, 2017.
- Alcon data on file, 2017.
- Alcon Data on File, 2020.
- Lee B, Chang D. Comparison of the rotational stability of two toric intraocular lenses in 1273 consecutive eyes. Ophthalmology. 2018;125(9):1325-1331.
- Alcon data on file, 2023.
- Alcon data on file, 2023.
- Clareon® PanOptix® Trifocal Hydrophobic Acrylic IOL Model CNWTT0 2021 Directions for Use.
- Clareon® Vivity® Extended Vision Hydrophobic IOL (CNWET0) Directions for Use – USA.